Breast-Conserving Surgery
(Breast Conservation Therapy, BCT, Lumpectomy, Segmental Mastectomy, Partial Mastectomy, Quadrantectomy)
Procedure overview
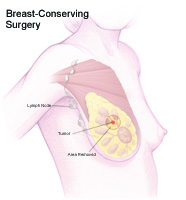
Breast-conserving surgery may be used as a part of a treatment plan for breast cancer. During breast-conserving surgery, the cancerous lump and a portion of the breast tissue around the cancerous lump are removed. However, the breast itself remains intact. The surgeon may also remove some of the lymph nodes under the arm to determine if the cancer has spread.
Lymph nodes are bean-shaped structures that drain fluid from the breast area, upper arms, the neck, and underarm regions. Often breast cancer spreads to these lymph nodes, thereby entering the lymphatic system and allowing the cancer to spread to other parts of the body.
Radiation therapy is often given after breast-conserving surgery to destroy cancer cells that may not have been removed during surgery. In some cases, chemotherapy and radiation are both given after breast-conserving surgery.
Anatomy of the breast
Each breast has 15 sections to 20 sections, called lobes, that are arranged like the petals of a daisy. Each lobe has many smaller lobules, which end in dozens of tiny bulbs that can produce milk.
The lobes, lobules, and bulbs are all linked by thin tubes called ducts. These ducts lead to the nipple in the center of a dark area of skin called the areola. Fat fills the spaces between lobules and ducts.
There are no muscles in the breast, but muscles lie under each breast and cover the ribs.
Each breast also contains blood vessels and vessels that carry lymph fluid. The lymph vessels lead to small bean-shaped organs called lymph nodes, clusters of which are found under the arm, above the collarbone, and in the chest, as well as in many other parts of the body.
Reasons for the procedure
Breast-conserving surgery is a treatment option for some women with small, localized breast cancers. Studies have shown that women who undergo breast-conserving surgery followed by radiation have similar overall survival rates as those who undergo mastectomy.
There may be other reasons for your doctor to recommend breast-conserving surgery.
In some cases, breast-conserving surgery may not be recommended as the treatment of choice. Reasons for not undergoing breast-conserving surgery may include, but are not limited to, the following:
-
Previous radiation therapy in the breast or chest area
-
Two or more cancerous areas present within the same breast
-
Tumor that is large relative to a smaller-sized breast
-
Connective tissue disease(s) that are sensitive to radiation therapy
-
Pregnancy at the time of radiation following surgery
-
Tumor size larger than 2 inches that does not decrease in size following chemotherapy
-
Residual tumor left over from previous breast-conserving surgery
Risks of the procedure
As with any surgical procedure, complications may occur. Some possible complications of breast-conserving surgery include, but are not limited to, the following:
-
Temporary swelling of the breast
-
Breast disfigurement (size and shape)
-
Hardness due to scar tissue that can form at the site of the incision
-
Wound infection or bleeding
-
Lymphedema or swelling of the arm due to lymph node removal. This is preceded by early symptoms, which include a feeling of tightness in the arm, pain, redness, and decreased flexibility of the arm, hand, and wrist.
Seroma (clear fluid trapped in a wound) is normally present after breast-conserving surgery. Troublesome seromas can be drained in a surgeon’s office and treated with compression or an injection that helps to harden the space in the breast if necessary.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
-
Your doctor will explain the procedure to you and offer you a chance to ask any questions that you might have about the procedure.
-
You will be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if something is not clear.
-
In addition to a complete medical history, your doctor may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may need to have blood tests or other diagnostic tests.
-
You will be asked to fast for 8 hours before the procedure, generally after midnight.
-
If you are pregnant or suspect that you may be pregnant, you should notify your health care provider.
-
Notify your doctor if you are sensitive to or are allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
-
Notify your doctor of all medications (prescription and over-the-counter) and herbal supplements that you are taking.
-
Notify your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. You may need to stop these medications prior to the procedure.
-
You may be given a sedative prior to the procedure to help you relax.
-
Based on your medical condition, your doctor may request other specific preparation.
During the procedure
Breast-conserving surgery may be performed on an outpatient basis or as part of your stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
Generally, breast-conserving surgery follows this process:
-
You will be asked to remove clothing and will be given a gown to wear.
-
An intravenous (IV) line may be started in your arm or hand.
-
You will be positioned on the operating table.
-
The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the procedure.
-
The skin over the surgical site will be cleansed with an antiseptic solution.
-
A small incision (cut) will be made over or near the breast tumor. The doctor will remove the lump or abnormality along with a portion of the surrounding breast tissue.
-
If the lymph nodes under the armpit are to be removed, a separate surgical incision may be made in or near the axilla (armpit).
-
Breast tissue and any other tissues that are removed will be sent to the lab for examination.
-
A drainage tube may be inserted into the affected area.
-
The skin will be closed with sutures or adhesive strips.
-
A sterile bandage or dressing will be placed over the site.
After the procedure
After the procedure, you will be taken to the recovery room for observation. Your recovery process will vary depending on the type of procedure performed and the type of anesthesia that is given. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room.
Generally, patients are able to go home the same day or within 1 day to 2 days following breast-conserving surgery.
Once you are home, it is important to keep the surgical area clean and dry. Your doctor will give you specific bathing instructions. If adhesive strips are used, they should be kept dry and generally will fall off within a few days.
The extent of pain depends on the amount and location of tissue that is removed during surgery. Soreness should decrease over time. Take a pain reliever for soreness as recommended by your doctor. Aspirin or certain other pain medications may increase the chance of bleeding. Be sure to take only recommended medications.
Your doctor may instruct you to wear a bra continuously for support for a period of time.
Normal activities can usually be resumed within 2 weeks. Meanwhile, you should avoid strenuous activities, particularly those that involve extensive use of the arm, such as cleaning windows or vacuuming for long periods. Your doctor will advise you about when you can start driving again and when you can return to work.
Breast-conserving surgery may be followed by radiation therapy. Your doctor will advise you about this depending on your particular situation.
Notify your doctor to report any of the following:
-
Fever and/or chills
-
Redness, swelling, or bleeding or other drainage from the incision site
-
Increased pain around the incision site
-
Swelling or numbness and/or tingling of the affected arm if lymph nodes have been removed
Arm care after lymph node removal
If lymph nodes are removed during breast-conserving surgery, the drainage of lymphatic fluid from the arm on the surgical side may be affected. Problems with lymphatic drainage may result in arm swelling and an increased risk for infection from trauma to the arm. In addition, there is an increased risk for blood clots in the blood veins of the armpit because of surgical trauma in the area.
Lifelong precautions to help prevent problems in the affected arm after lymph node dissection include, but are not limited to:
-
No needle sticks or IV insertions in the affected arm
-
No blood pressure measurements in the affected arm
-
Follow instructions regarding exercises of the arms carefully
-
Avoid injuries, such as scratches or splinters, to the affected arm
-
Elevate the arm, with the hand above the elbow, to assist with drainage of lymphatic fluid
-
Wear gloves when gardening or performing any activity in which there is a risk for skin puncture of the fingers and/or hands, or when using strong or harsh chemicals such as detergents or household cleaners
-
Avoid sunburns
-
Use an electric shaver rather than a razor with a blade to shave under the arm
-
Avoid any constrictive items on the affected arm, such as elastic cuffs or tight watches or other jewelry
-
Use the unaffected arm to carry heavy packages, bags, or purses
-
Avoid insect bites or stings by using insect repellents and/or wearing long sleeves
Your doctor may give you additional or alternate instructions after the procedure, depending on your particular situation.
Schedule a Mamogram at Richmond University Medical Center
Early detection and treatment is the best strategy for a better cancer outcome. Schedule your mamogram at RUMC: Call 718-818-3280.
Kathy Giovinazzo is Director of Radiology at Richmond University Medical Center.
For More Information
For more information or to schedule an appointment, contact Dr. Thomas Forlenza at 718-816-4949. His office is located at 1366 Victory Blvd on Staten Island.
Dr. Forlenza is the Director of Oncology at Richomd University Medical Center