Tests That Help Evaluate Lung Cancer
Your doctor took a biopsy to know if you have cancer. He or she took a sample of cells from either your lung or the surrounding fluids.
Your doctor may request more tests. The goal is to learn more about your specific type of cancer and its specific location. These details help your doctor decide on the treatment that is likely to be most effective for you. Here are some of the tests you may need to have.
Bone scan
A bone scan is one kind of radionuclide scanning. This test is done mainly when there is reason to think the cancer may have spread to your bones. For this test, you'll be injected with a small amount of a radioactive substance. It travels through the bloodstream and collects in areas of abnormal bone growth. Regardless of which type of lung cancer you have, you may not need a bone scan if you have already had a positron emission tomography (PET) scan, which can often show the same type of results.
Bone marrow biopsy
This test is not nearly as common as some of the others, but it may be required in rare instances. To do this test, your doctor inserts a hollow needle through your skin into your hip bone. The doctor moves the needle around to force a tiny sample of bone marrow inside it. You'll get a local anesthetic first to numb the skin. You may still feel a brief sharp pain.
CT scan
During a CT scan — often called a CAT scan or spiral CT scan — X-rays scan a part of the body (such as the chest or abdomen) in about 15 to 25 seconds. When you have lung cancer, these pictures help your doctor see where the cancer is in your chest. They also show whether the cancer has spread to your lymph nodes, liver, or adrenal glands, which rest on top of your kidneys. To have the test, you lie still on a table as it gradually slides through the center of the CT scanner. A computer uses the data from the X-rays to create many detailed pictures of your chest. A CT scan is painless. You may be asked to hold your breath one or more times during the scan. In some cases, you get an IV drip with a contrast medium a few hours before the scan. This helps your lungs show up better during the scan. You may be asked not to eat anything, called fasting, in the time between drinking the contrast and the scan. The contrast will gradually pass through your system and exit through your bowel movements.
Magnetic resonance imaging (MRI)
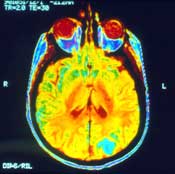
An MRI may be used to determine if cancer has spread to your chest or brain. If it has, an MRI can also show the size and extent of the spread. Your doctor may also request an MRI if the results of an X-ray or CT scan don't clearly give the answer. In some cases, you are injected with a contrast dye right before getting the scan. For this test, you lie still on a table as it passes through a scanner. A computer uses the data from the magnetic waves to create very detailed pictures of the inside of your body. Each image may take 2 to 15 minutes, so the whole experience may take an hour or more. These pictures can show the difference between normal and diseased tissue. This test is painless. Ask for earplugs since there is a loud thumping noise during the scan. If you are claustrophobic, you may need a sedative before having this test.
Endobronchial ultrasound
This is a test to look for enlarged lymph nodes or other problems in the mediastinum (the area between the lungs). For this test, a bronchoscope is fitted with an ultrasound transducer at its tip and is passed down into the windpipe. You may be sedated or asleep (under general anesthesia) for this test.
The transducer emits sound waves and picks up the echoes as they bounce off body tissues. The echoes are converted by a computer into a black and white image that is displayed on a computer screen. The transducer can be pointed in different directions to look at lymph nodes and other structures in the mediastinum. If suspicious areas (such as enlarged lymph nodes) are seen on the ultrasound, a hollow needle can be passed through the bronchoscope to get biopsy samples of them. The samples are then sent to a lab to be looked at under a microscope.
A similar test, known as endoscopic esophageal ultrasound, can also be used to look at lymph nodes in the mediastinum. But for this test, the scope is passed down the esophagus instead of the windpipe.
Mediastinoscopy
Your doctor may suggest this test to evaluate the status of the lymph nodes in your chest. Although an imaging test, such as a CT scan, may show if there are enlarged lymph nodes, the pathologist needs to find out if they have cancer in them. This is a test done by a surgeon. For this test, you get an anesthetic that puts you to sleep so you don't feel anything. Your doctor may make a small cut in the front of your neck. Or your doctor may make a small cut in your chest. The doctor then uses a lighted scope with a small video camera on the end to look at the center of your chest, called the mediastinum, and the lymph nodes there. The doctor uses the scope to remove some tissue. The cells removed from the lymph nodes are sent to the lab to be checked for cancer.
Positron emission tomography scan (PET scan)
A PET scan can help your doctor know if cancer has spread. Because it scans your whole body, your doctor may order a PET scan instead of ordering multiple X-rays of different places on your body. For this test, you either swallow or get injected with a chemical. It may be glucose that carries a mildly radioactive substance. It may take a few hours to more than a day for the chemical to reach the targeted organ. Then, you'll lie still on a table that is pushed into the PET scanner, which rotates around you, taking pictures of where the glucose is being used in the body. Tumors are more active and use more glucose than healthy cells. A PET scan is painless and noninvasive. Some people are sensitive to the glucose and may have nausea, headaches, or vomiting.
Some cancer centers have new technology that combines a PET scan with a CT scan. The result is a more precise image of where the cancer is located.
For More Information
For more information on how to quit smoking or schedule lung cancer screenings, contact Nancy Sayegh-Rooney, R.N., Pulmonary Nurse Navigator at Richmond University Medical Center, 718-818-2391.
Free screenings are available for at-risk individuals, please call for additional information.